Pleurodesis
What is Pleurodesis?
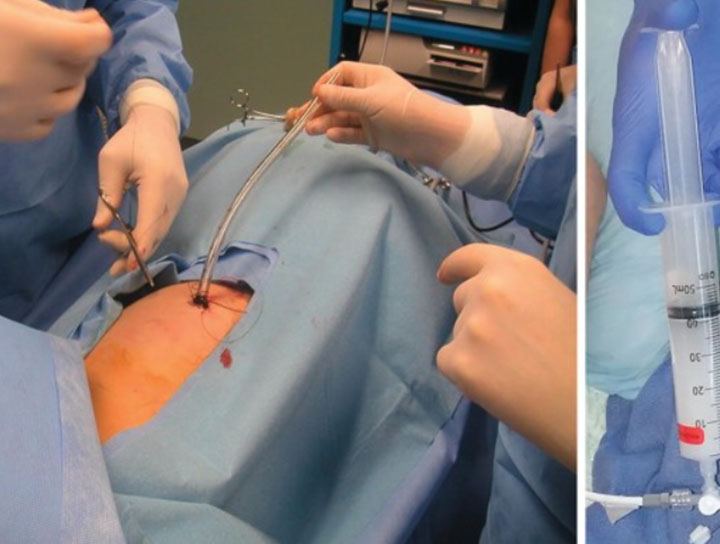
Pleurodesis aims to obliterate the pleural space by producing extensive adhesion of the visceral and parietal pleura, in order to control relapse of either pleural effusions (mostly malignant) or pneumothorax. This procedure is particularly beneficial for patients who experience recurrent pleural effusions or pneumothorax that significantly affects their quality of life.
Mechanism of Action
A tight and complete apposition between the two pleural layers is a necessary condition to obtain a successful pleurodesis. Besides this mechanical aspect, there are many biological mechanisms that appear to be common to most of the sclerosing agents currently used. Following intrapleural application of the sclerosing agent, the following processes occur in the pleural space:
- Diffuse inflammation
- Pleural coagulation-fibrinolysis imbalance (favoring the formation of fibrin adhesions)
- Recruitment and subsequent proliferation of fibroblasts
- Collagen production
The pleural mesothelial lining is the primary target for the sclerosant and plays a pivotal role in the whole pleurodesis process, including the release of several mediators like interleukin-8, transforming growth factor-β, and basic fibroblast growth factor.
Factors Affecting Success
When the tumor burden is high, normal mesothelial cells are scarce, leading to a decreased response to the sclerosing agent and potential failure of pleurodesis. Additionally, the type of tumor in the pleural cavity may also affect the outcome of pleurodesis, with diffuse malignant mesothelioma and metastatic lung carcinomas showing a poorer response.
Sclerosing Agents
There is general agreement that talc obtains the best results among the various sclerosing agents. Preliminary experimental studies suggest that talc can induce apoptosis in tumor cells and inhibit angiogenesis, thus contributing to better control of malignant pleural effusion.
However, there are concerns about complications associated with talc and other agents, particularly related to systemic inflammation and possible activation of the coagulation cascade. To prevent extrapleural talc dissemination, large-particle talc is recommended.
Prophylactic Measures
Although large-particle talc could interfere with the mechanisms leading to pleurodesis, a carefully balanced clinical decision must be made. Prophylactic treatment with subcutaneous heparin is recommended during hospitalization, immediately before and after the pleurodesis procedure, to mitigate the risk of thromboembolic events.
Conclusion
Pleurodesis is a valuable procedure for managing recurrent pleural effusions and pneumothorax. Understanding the mechanisms, factors affecting success, and appropriate use of sclerosing agents can optimize outcomes for patients undergoing this intervention.
