EBUS TBNA
EBUS TBNA
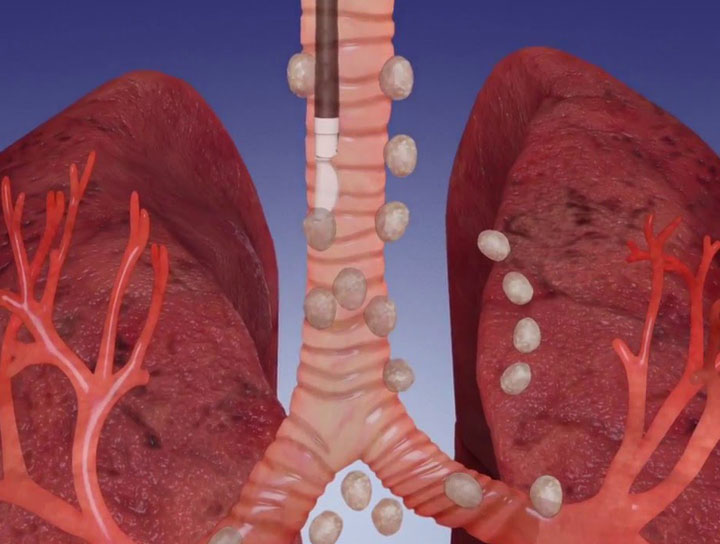
Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) has recently emerged as a minimally invasive and safe modality for the evaluation of mediastinal lymphadenopathy, particularly in staging of lung carcinoma patients. In high tuberculosis endemic countries, EBUS-TBNA is useful in obtaining tissue diagnosis of granulomatous inflammation. Role of EBUS-TBNA in workup of extrapulmonary malignancies is not widely described. Herein, a brief overview of importance of EBUS-TBNA in investigation of extrapulmonary lesions/malignancies is presented.
Mediastinoscopy vs EBUS-TBNA
Mediastinoscopy is the gold standard technique for mediastinal staging in patients with pulmonary and extrapulmonary malignancy (EPM); however, it is limited by invasiveness of the procedure, requirement of general anesthesia, and increased risk of mortality and morbidity. Mediastinoscopy is also a technically challenging procedure and fraught with considerable postoperative mediastinal fibrosis which complicates reexplorations.
Conventional transbronchial needle aspiration (TBNA), although safer, is a “blind” procedure used for sampling only large subcarinal/right paratracheal lymph nodes.
In contrast, endobronchial ultrasound (EBUS)-guided needle aspiration technique is minimally invasive, safe, and performed under local anesthesia and allows real-time sampling of small mediastinal nodes inaccessible by other modalities.
Clinical Applications
Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) has been extensively used for the nodal staging of lung cancer with a high yield and superior sensitivity to mediastinoscopy. However, in a small proportion (~10–16%) of cases, EBUS-TBNA is indicated for evaluation of mediastinal masses in patients with known/suspected EPMs. Extrapulmonary lesions diagnosed on EBUS-TBNA are most frequently either metastases from EPM or granulomatous inflammation or other infective pathology.
Mediastinal and hilar lymphadenopathy are common findings on imaging in patients with EPMs. They may indicate distant metastasis in a newly diagnosed patient, disease relapse, second primary malignancy, or granulomatous disease in a previously diagnosed and treated patient, may be the first sign of malignancy in an occult EPM, or may be reactive lymphoid hyperplasia. Patients with EPMs who develop lung metastasis, coexistent mediastinal, or hilar lymphadenopathy are seen in nearly a third of these cases.
Importance of Diagnosis
Confirmation of lymph node metastases is important in these patients as it worsens prognosis. Lung metastasectomy is not beneficial in patients with metastatic lymph nodes.
Role of EBUS-TBNA in sampling mediastinal lymph nodes and masses in patients with EPMs has been evaluated in a few clinical studies previously, with variable sensitivities (81–95%) and negative predictive values (NPV) reported. Metastases are found in half of these cases, whereas a quarter of them harbor a second primary malignancy, most commonly in the lung. Most importantly, a significant proportion of patients are found to have granulomatous inflammation such as tuberculosis and sarcoidosis.
Conclusion
In conclusion, EBUS-TBNA is a sensitive, specific, minimally invasive, and safe procedure for the correct diagnosis of mediastinal and hilar lesions or lymphadenopathies in patients with EPM. It has been observed in prior studies that EBUS-TBNA results alter treatment procedures in over half of cases and obviate invasive surgical procedures in 60–87% of patients with EPM. The positive predictive value of EBUS-TBNA for malignancy is nearly 100%, and patients usually do not require further workup, except when EBUS-TBNA material is inadequate for proper characterization or biomarker testing.
